![]()
Editor's note: A longer version of this article was first published on Medium on March 20, 2020. It is being reposted with the author's permission. Watch and read the transcript of his interview with Rappler's Maria Ressa.
READ: Conclusion | [ANALYSIS] COVID-19: The hammer and the dance
Strong coronavirus measures today should only last a few weeks, there shouldn’t be a big peak of infections afterwards, and it can all be done for a reasonable cost to society, saving millions of lives along the way. If we don’t take these measures, tens of millions will be infected, many will die, along with anybody else that requires intensive care, because the healthcare system will have collapsed.
Since my first article published on March 10, the conversation has changed and many countries have taken measures. Here are some of the most illustrative examples:
Measures in Spain and France
In one extreme, we have Spain and France. This is the timeline of measures for Spain:
On Thursday, March 12, the President dismissed suggestions that the Spanish authorities had been underestimating the health threat.
On Friday, they declared the State of Emergency.
On Saturday, measures were taken:
- People can’t leave home except for key reasons: groceries, work, pharmacy, hospital, bank or insurance company (extreme justification).
- Specific ban on taking kids out for a walk or seeing friends or family (except to take care of people who need help, but with hygiene and physical distance measures).
- All bars and restaurants closed. Only take-home acceptable.
- All entertainment closed: sports, movies, museums, municipal celebrations.
- Weddings can’t have guests. Funerals can’t have more than a handful of people.
- Mass transit remains open.
On Monday, land borders were shut.
Some people see this as a great list of measures. Others put their hands up in the air and cry of despair. This difference is what this article will try to reconcile.
France’s timeline of measures is similar, except they took more time to apply them, and they are more aggressive now. For example, rent, taxes and utilities are suspended for small businesses.
Measures in the US and UK
The US and UK, like countries such as Switzerland or Netherlands, have dragged their feet in implementing measures. Here’s the timeline for the US:
- Wednesday, March 11: travel ban.
- Friday: National Emergency declared. No social distancing measures.
- Monday: the government urges the public to avoid restaurants or bars and attend events with more than 10 people. No social distancing measure is actually enforceable. It’s just a suggestion.
Lots of states and cities are taking the initiative and mandating much stricter measures.
The UK has seen a similar set of measures: lots of recommendations, but very few mandates.
These two groups of countries illustrate the two extreme approaches to fight the coronavirus: mitigation and suppression. Let’s understand what they mean.
Before we do that, let’s see what doing nothing would entail for a country like the US.
Option 1: Do nothing
![]()
This fantastic epidemic calculator can help you understand what will happen under different scenarios. I’ve pasted below the graph the key factors that determine the behavior of the virus. Note that infected, in pink, peak in the tens of millions at a certain date. Most variables have been kept from the default. The only material changes are R from 2.2 to 2.4 (corresponds better to currently available information. See at the bottom of the epidemic calculator), fatality rate (4% due to healthcare system collapse. See details below or in the previous article), length of hospital stay (down from 20 to 10 days) and hospitalization rate (down from 20% to 14% based on severe and critical cases. Note the WHO calls out a 20% rate) based on our most recently available gathering of research. Note that these numbers don’t change results much. The only change that matters is the fatality rate.
If we do nothing: Everybody gets infected, the healthcare system gets overwhelmed, the mortality explodes, and ~10 million people die (blue bars). For the back-of-the-envelope numbers: if ~75% of Americans get infected and 4% die, that’s 10 million deaths, or around 25 times the number of US deaths in World War II.
You might wonder: “That sounds like a lot. I’ve heard much less than that!”
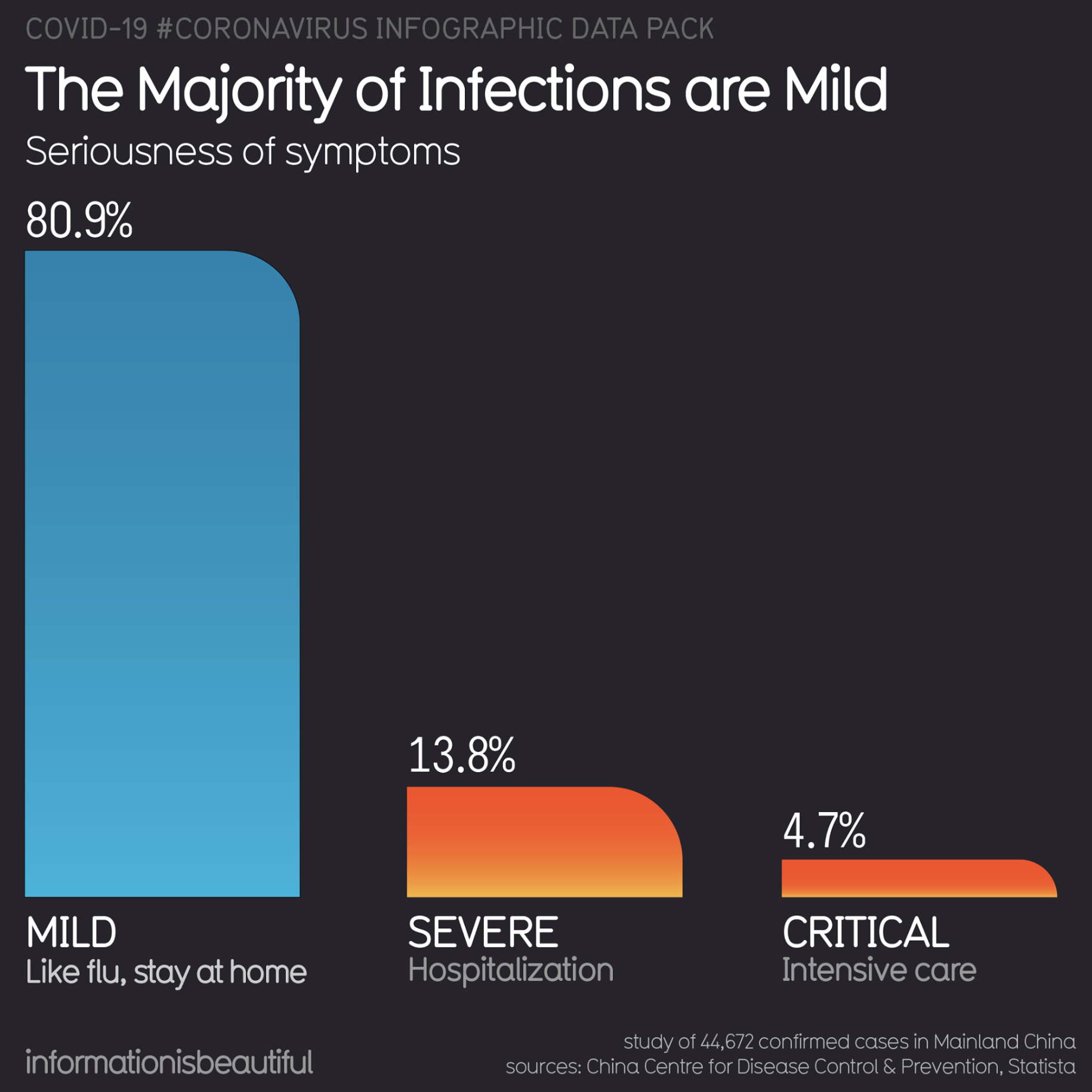
So what’s the catch? With all these numbers, it’s easy to get confused. But there’s only two numbers that matter: What share of people will catch the virus and fall sick, and what share of them will die. If only 25% are sick (because the others have the virus but don’t have symptoms so aren’t counted as cases), and the fatality rate is 0.6% instead of 4%, you end up with 500,000 deaths in the US. Still massive. But 20 times less than above.
The fatality rate is crucial, so let’s understand it better. What really causes the coronavirus deaths?
How should we think about the fatality rate?
This is the same graph as before, but now looking at hospitalized people instead of infected and dead:
![]()
The light blue area is the number of people who would need to go to the hospital, and the darker blue represents those who need to go to the intensive care unit (ICU). You can see that number would peak at above 3 million.
Now compare that to the number of ICU beds we have in the US (50,000 as of writing, we could double that repurposing other space). That’s the red dotted line.
No, that’s not an error.
That red dotted line is the capacity we have of ICU beds. Everyone above that line would be in critical condition but wouldn’t be able to access the care they need, and would likely die.
Instead of ICU beds you can also look at ventilators, but the result is broadly the same, since there are fewer than 100,000 ventilators in the US.
As of writing, at least one Seattle hospital is unable to intubate patients over 65 due to shortages of equipment and gives them a 90% chance of dying.
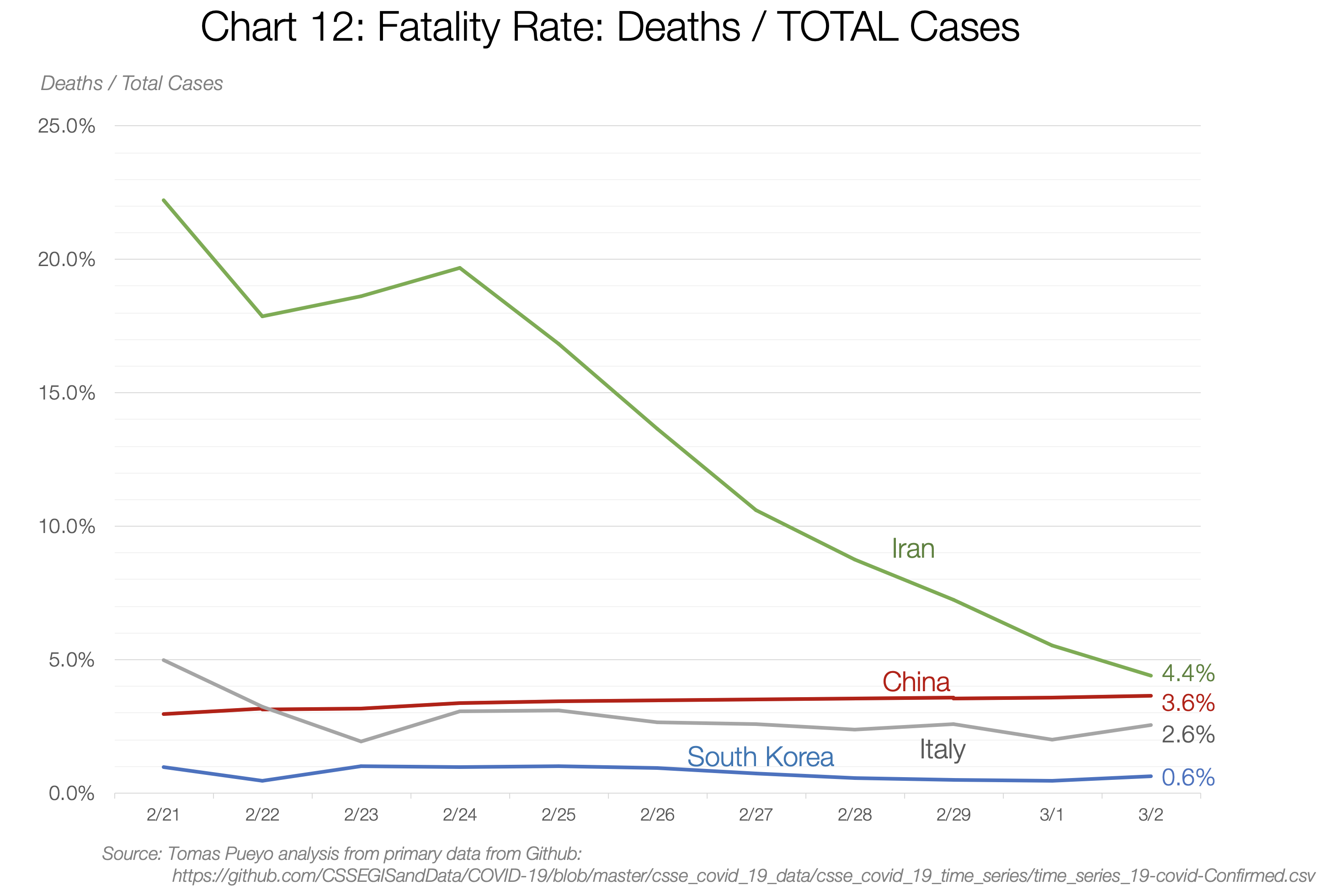
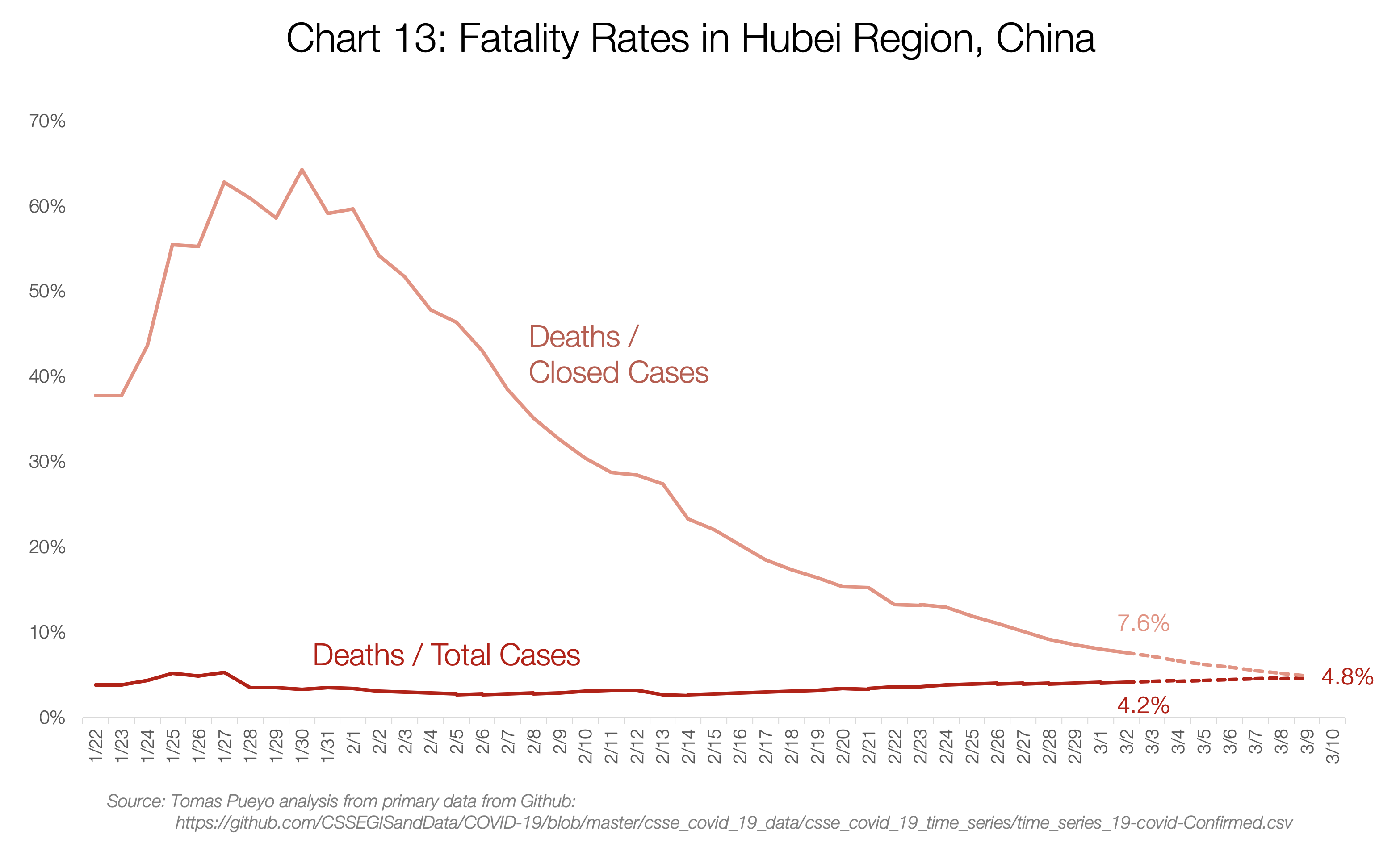
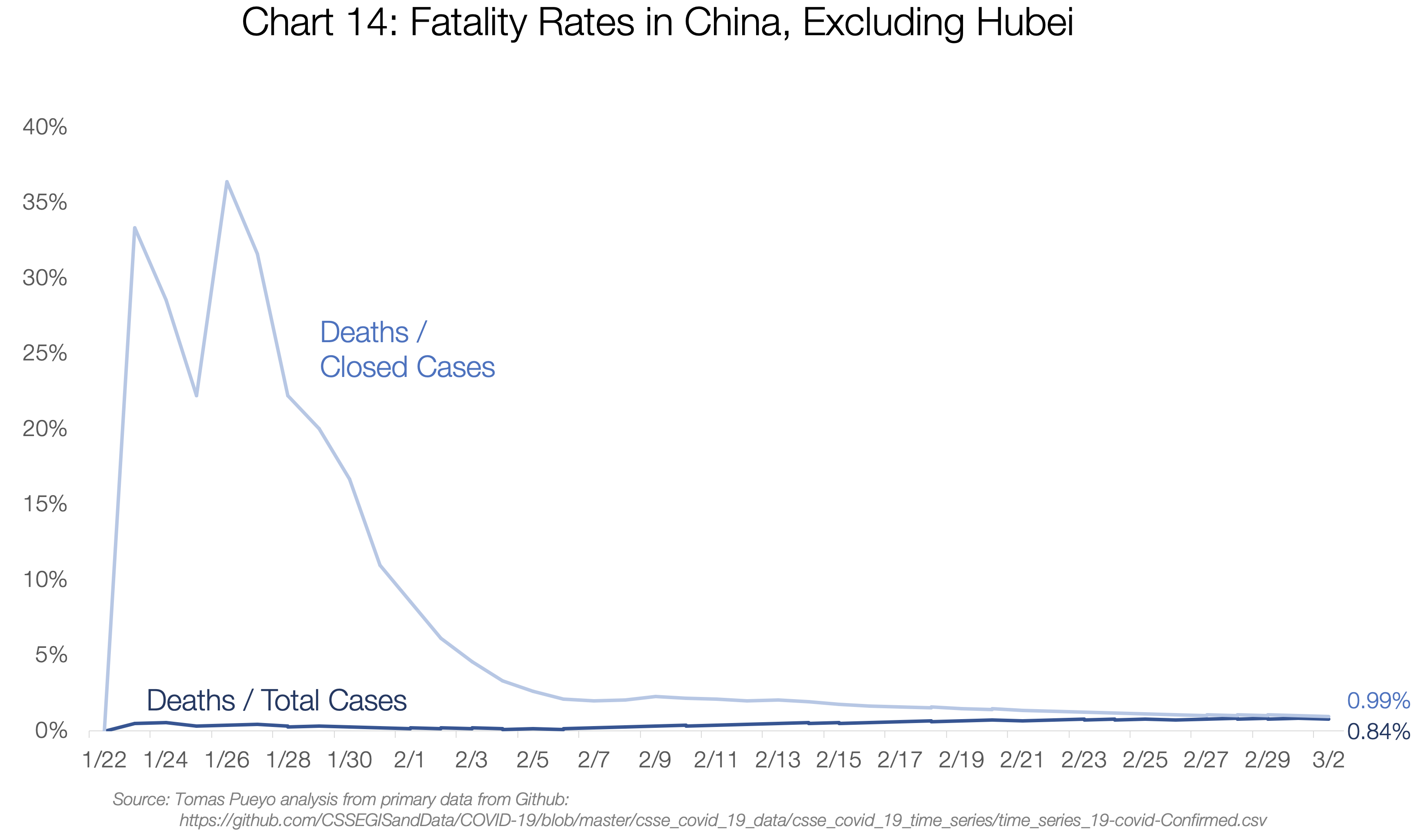
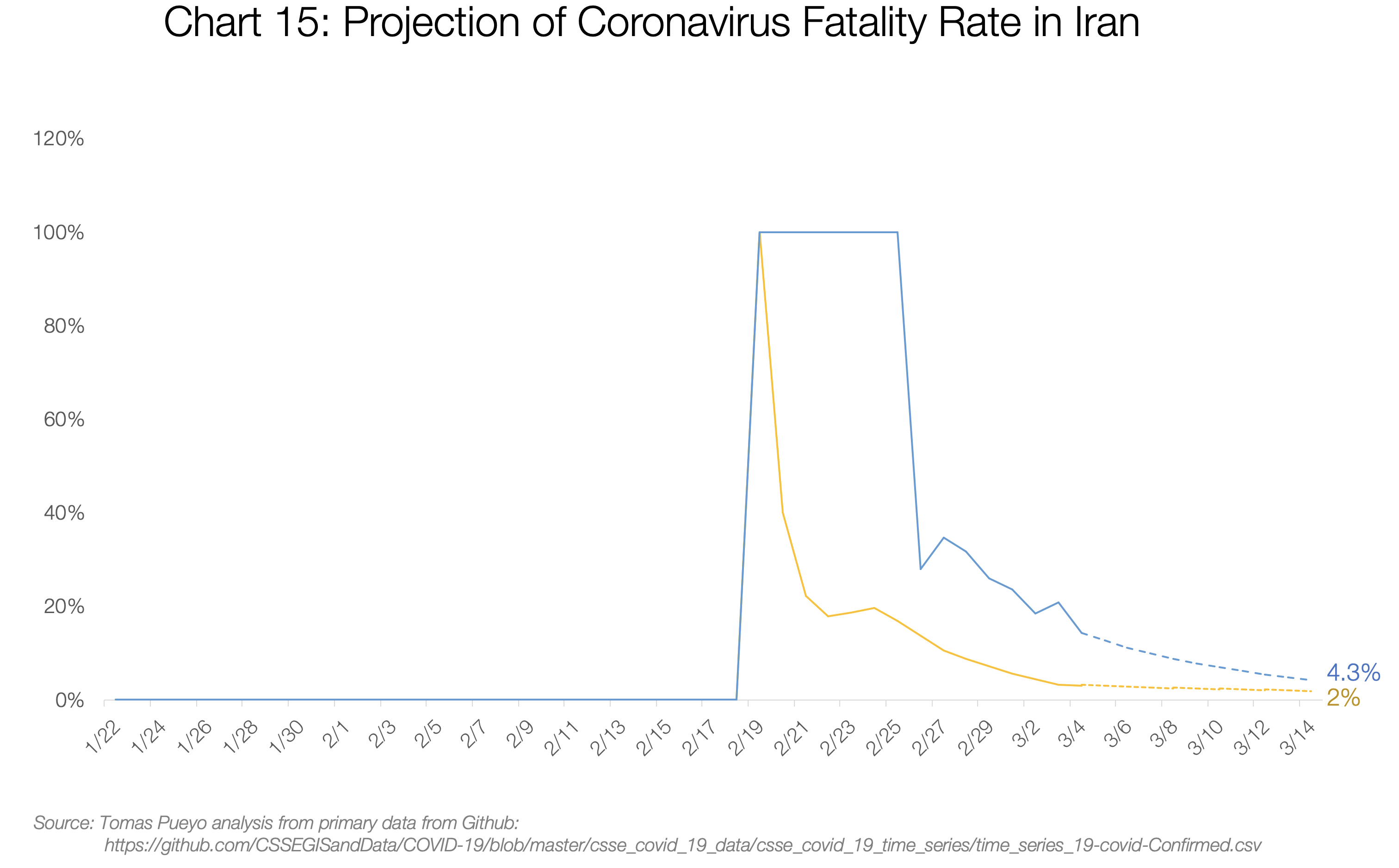
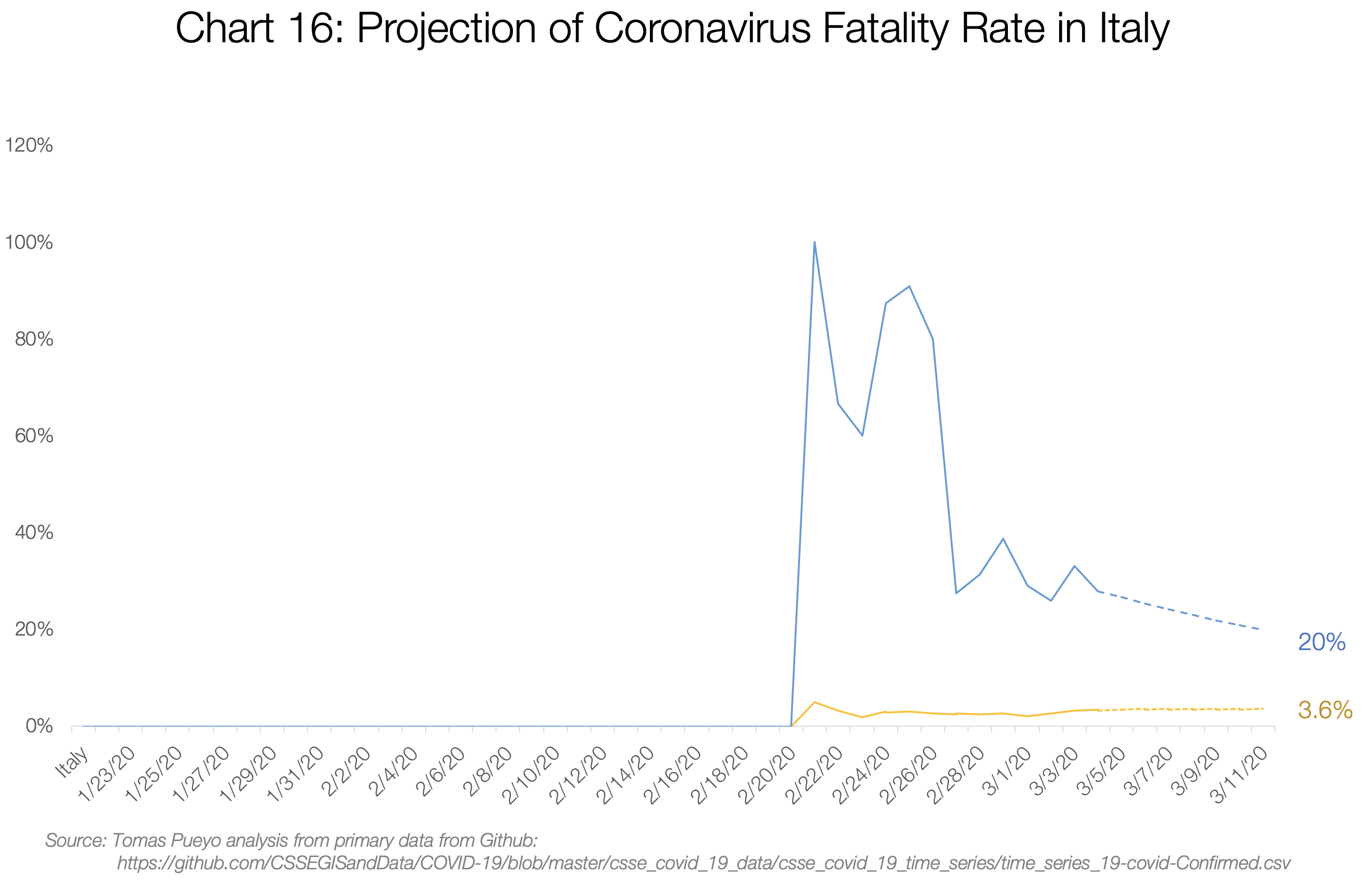
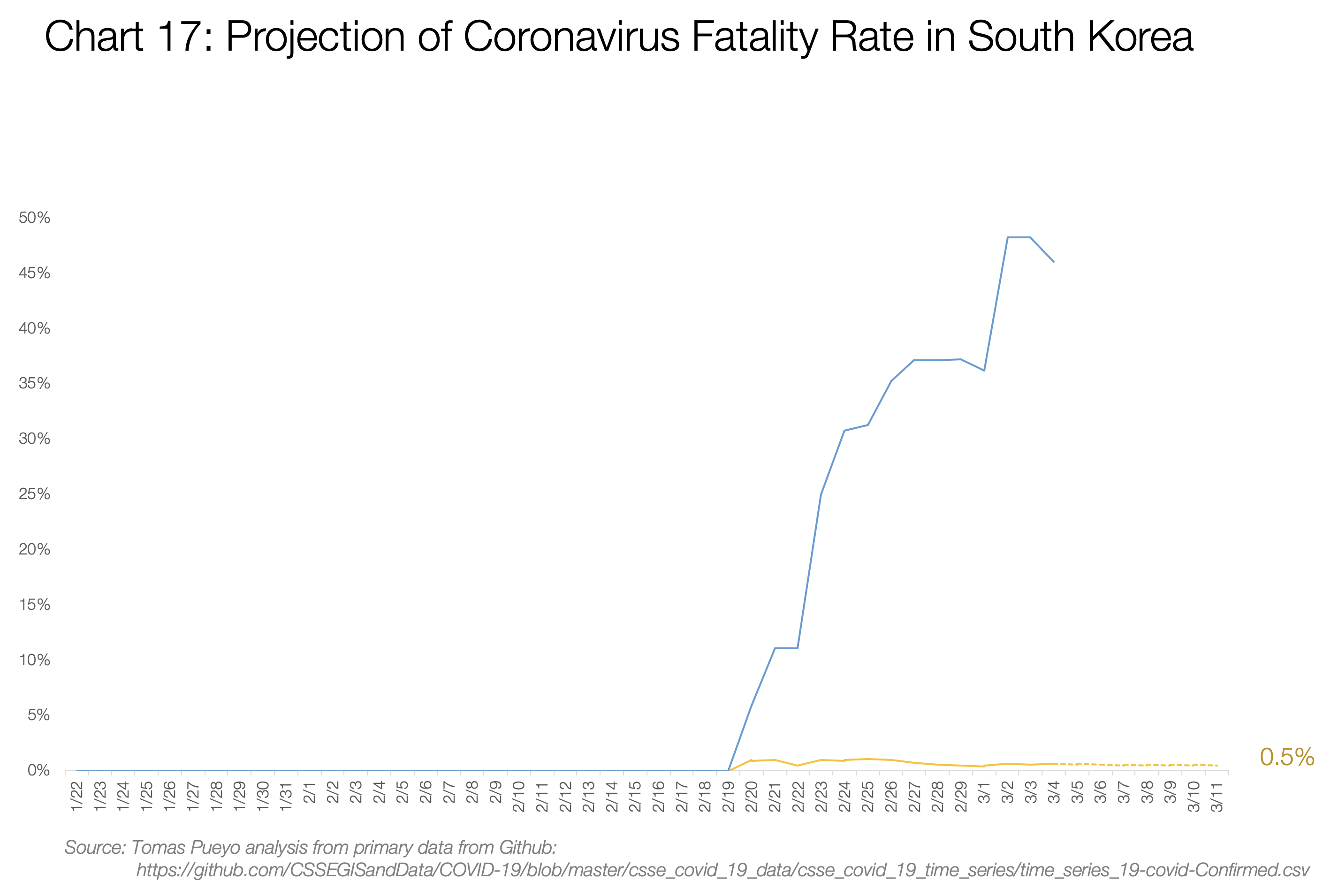
This is why people died in droves in Hubei and are now dying in droves in Italy and Iran. The Hubei fatality rate ended up better than it could have been because they built two hospitals nearly overnight. Italy and Iran can’t do the same: few, if any, other countries can. We’ll see what ends up happening there.
So why is the fatality rate close to 4%?
If 5% of your cases require intensive care and you can’t provide it, most of those people die. As simple as that.
Additionally, recent data suggests that US cases are more severe than in China. I wish that was it, but it isn’t.
Collateral damage
These numbers only show people dying from coronavirus. But what happens if all your healthcare system is collapsed by coronavirus patients? Others also die from other ailments.
What happens if you have a heart attack but the ambulance takes 50 minutes to come instead of 8 (too many coronavirus cases) and once you arrive, there’s no ICU and no doctor available? You die.
There are 4 million admissions to the ICU in the US every year, and 500,000 (~13%) of them die. Without ICU beds, that share would likely go much closer to 80%. Even if only 50% died, in a year-long epidemic you go from 500,000 deaths a year to 2 million, so you’re adding 1.5 million deaths, just with collateral damage.
If the coronavirus is left to spread, the US healthcare system will collapse, and the deaths will be in the millions, maybe more than 10 million.
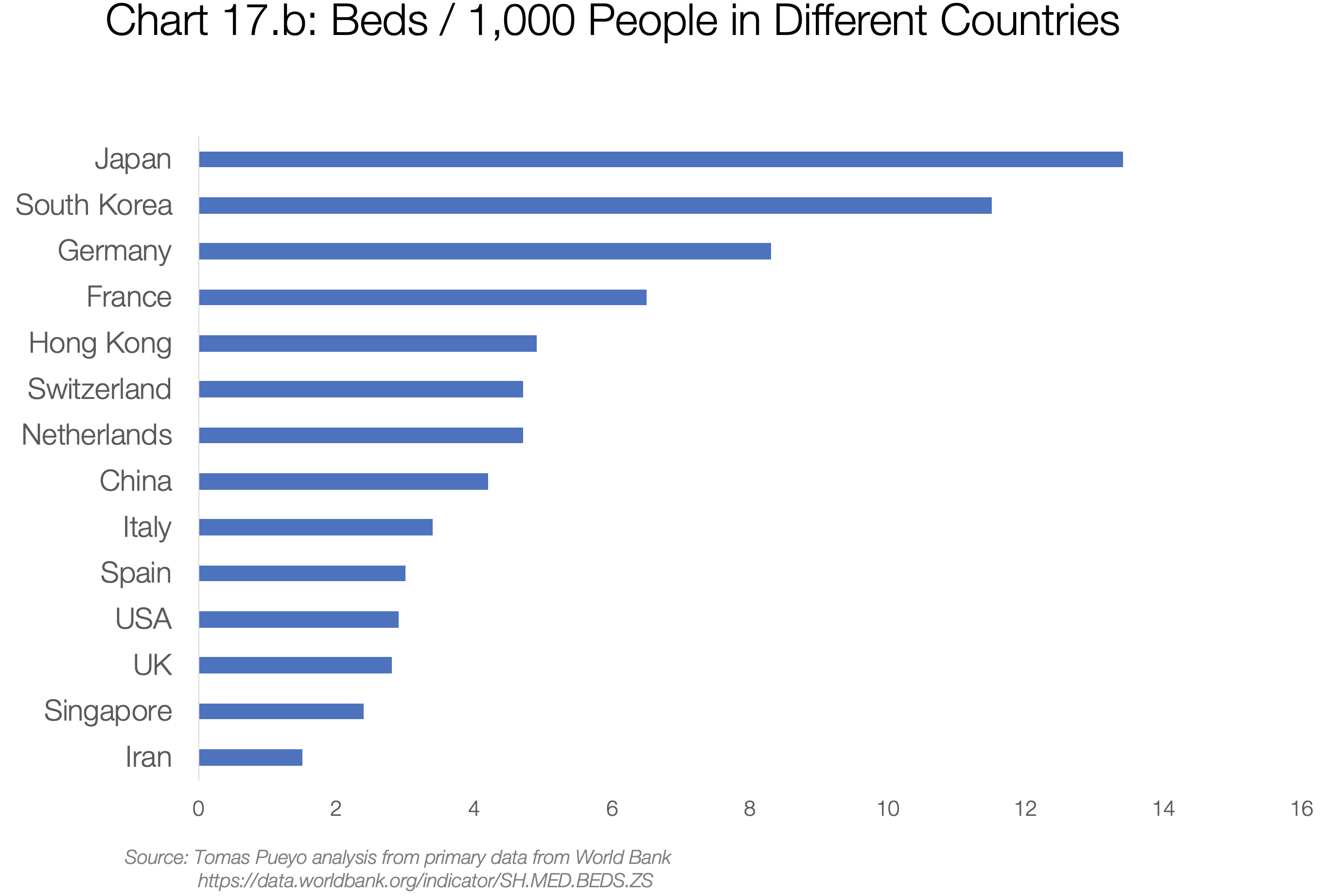
The same thinking is true for most countries. The number of ICU beds and ventilators and healthcare workers are usually similar to the US or lower in most countries. Unbridled coronavirus means healthcare system collapse, and that means mass death.
Option 2: Mitigation strategy
By now, I hope it’s pretty clear we should act. The two options that we have are mitigation and suppression.
Mitigation goes like this: “It’s impossible to prevent the coronavirus now, so let’s just have it run its course, while trying to reduce the peak of infections. Let’s just flatten the curve a little bit to make it more manageable for the healthcare system.”
![]()
This chart appears in a very important paper published by the Imperial College London. Apparently, it pushed the UK and US governments to change course.
It’s a very similar graph as the previous one. Not the same, but conceptually equivalent. Here, the “Do nothing” situation is the black curve. Each one of the other curves are what would happen if we implemented tougher and tougher social distancing measures. The blue one shows the toughest social distancing measures: isolating infected people, quarantining people who might be infected, and secluding old people. This blue line is broadly the current UK coronavirus strategy, although for now they’re just suggesting it, not mandating it.
Here, again, the red line is the capacity for ICUs, this time in the UK. Again, that line is very close to the bottom. All that area of the curve on top of that red line represents coronavirus patients who would mostly die because of the lack of ICU resources.
Not only that, but by flattening the curve, the ICUs will collapse for months, increasing collateral damage.
You should be shocked. When you hear, “We’re going to do some mitigation,” what you should really hear is, “We will knowingly overwhelm the healthcare system, driving the fatality rate up by a factor of 10 times at least.”
You would imagine this is bad enough. But we’re not done yet. Because one of the key assumptions of this strategy is what’s called “herd immunity."
Herd immunity and virus mutation
The idea is that all the people who are infected and then recover are now immune to the virus. This is at the core of this strategy: “Look, I know it’s going to be hard for some time, but once we’re done and a few million people die, the rest of us will be immune to it, so this virus will stop spreading and we’ll say goodbye to the coronavirus. Better do it at once and be done with it, because our alternative is to do social distancing for up to a year or risk having this peak happen later anyways.”
Except this assumes one thing: the virus doesn’t change too much. If it doesn’t change much, then lots of people do get immunity, and at some point the epidemic dies down.
How likely is this virus to mutate? It already has.
China has already seen two strains of the virus: the S and the L. The S was focused in Hubei and deadlier, but the L was the one that spread through the world.
Not only that, but this virus continues to mutate.
![]()
This graph represents the different mutations of the virus. You can see that the initial strains started in purple in China, but then they started mutating. The strains in Europe are mostly green and yellow families, while the US is seeing a different family in red. As more time passes, more of these strains will start appearing.
This should not be surprising: RNA-based viruses like the coronavirus or the flu tend to mutate around 100 times faster than DNA-based ones – although the coronavirus mutates more slowly than influenza viruses.
Not only that, but the best way for this virus to mutate is to have millions of opportunities to do so, which is exactly what a mitigation strategy would provide: hundreds of millions of people infected.
That’s why you have to get a flu shot every year. Because there are so many flu strains, with new ones always evolving, the flu shot can never protect against all strains.
Put in another way: the mitigation strategy not only assumes millions of deaths for a country like the US or the UK. It also gambles on the fact that the virus won’t mutate too much – which we know it does. And it will give it the opportunity to mutate. So once we’re done with a few million deaths, we could be ready for a few million more — every year. This corona virus could become a recurring fact of life, like the flu, but many times deadlier.
The best way for this virus to mutate is to have millions of opportunities to do so, which is exactly what a mitigation strategy would provide.
So if neither doing nothing and mitigation will work, what’s the alternative? It’s called suppression.
Option 3: Suppression strategy
The mitigation strategy doesn’t try to contain the epidemic, just flatten the curve a bit. Meanwhile, the suppression strategy tries to apply heavy measures to quickly get the epidemic under control. Specifically:
- Go hard right now. Order heavy social distancing. Get this thing under control.
- Then, release the measures, so that people can gradually get back their freedoms and something approaching normal social and economic life can resume.
What does that look like?
![]()
All the model parameters are the same, except that there is an intervention around now to reduce the transmission rate to R=0.62, and because the healthcare system isn’t collapsed, the fatality rate goes down to 0.6%. I defined “around now” as having ~32,000 cases when implementing the measures (3x the official number as of today, 3/19). Note that this is not too sensitive to the R chosen. An R of 0.98 for example shows 15,000 deaths. Five times more than with an R of 0.62, but still tens of thousands of deaths and not millions. It’s also not too sensitive to the fatality rate: if it’s 0.7% instead of 0.6%, the death toll goes from 15,000 to 17,000. It’s the combination of a higher R, a higher fatality rate, and a delay in taking measures that explodes the number of fatalities. That’s why we need to take measures to reduce R today. For clarification, the famous R0 is R at the beginning (R at time 0). It’s the transmission rate when nobody is immune yet and there are no measures against it taken. R is the overall transmission rate.
Under a suppression strategy, after the first wave is done, the death toll is in the thousands, and not in the millions.
Why? Because not only do we cut the exponential growth of cases. We also cut the fatality rate since the healthcare system is not completely overwhelmed. Here, I used a fatality rate of 0.9%, around what we’re seeing in South Korea today, which has been most effective at following a suppression strategy.
Said like this, it sounds like a no-brainer. Everybody should follow the suppression strategy.
So why do some governments hesitate?
They fear 3 things:
- This first lockdown will last for months, which seems unacceptable for many people.
- A months-long lockdown would destroy the economy.
- It wouldn’t even solve the problem, because we would be just postponing the epidemic: later on, once we release the social distancing measures, people will still get infected in the millions and die.
Here is how the Imperial College team modeled suppressions. The green and yellow lines are different scenarios of suppression. You can see that doesn’t look good: We still get huge peaks, so why bother?
![]()
We’ll get to these questions in a moment, but there’s something more important before.
This is completely missing the point.
Presented like these, the two options of mitigation and suppression, side by side, don’t look very appealing. Either a lot of people die soon and we don’t hurt the economy today, or we hurt the economy today, just to postpone the deaths.
This ignores the value of time.
The value of time
In our previousposts, we explained the value of time in saving lives. Every day, every hour we waited to take measures, this exponential threat continued spreading. We saw how a single day could reduce the total cases by 40% and the death toll by even more.
But time is even more valuable than that.
We’re about to face the biggest wave of pressure on the healthcare system ever seen in history. We are completely unprepared, facing an enemy we don’t know. That is not a good position for war.
What if you were about to face your worst enemy, of which you knew very little, and you had two options: either you run towards it, or you escape to buy yourself a bit of time to prepare. Which one would you choose?
This is what we need to do today. The world has awakened. Every single day we delay the coronavirus, we can get better prepared. The next sections detail what that time would buy us:
Lower the number of cases
With effective suppression, the number of true cases would plummet overnight, as we saw in Hubei last week.
![]()
As of today, there are zero daily new cases of coronavirus in the entire 60 million-big region of Hubei.
The diagnostics would keep going up for a couple of weeks, but then they would start going down. With fewer cases, the fatality rate starts dropping too. And the collateral damage is also reduced: fewer people would die from non-coronavirus-related causes because the healthcare system is simply overwhelmed.
Suppression would get us:
- Fewer total cases of coronavirus
- Immediate relief for the healthcare system and the humans who run it
- Reduction in fatality rate
- Reduction in collateral damage
- Ability for infected, isolated, and quarantined healthcare workers to get better and back to work. In Italy, healthcare workers represent 8% of all contagions.
Understand the true problem: Testing and tracing
Right now, the UK and the US have no idea about their true cases. We don’t know how many there are. We just know the official number is not right, and the true one is in the tens of thousands of cases. This has happened because we’re not testing, and we’re not tracing.
- With a few more weeks, we could get our testing situation in order, and start testing everybody. With that information, we would finally know the true extent of the problem, where we need to be more aggressive, and what communities are safe to be released from a lockdown.
- New testing methods could speed up testing and drive costs down substantially.
- We could also set up a tracing operation like the ones they have in China or other East Asia countries, where they can identify all the people that every sick person met, and can put them in quarantine. This would give us a ton of intelligence to release later on our social distancing measures: if we know where the virus is, we can target these places only. This is not rocket science: it’s the basics of how East Asia countries have been able to control this outbreak without the kind of draconian social distancing that is increasingly essential in other countries.
The measures from this section (testing and tracing) single-handedly curbed the growth of the coronavirus in South Korea and got the epidemic under control, without a strong imposition of social distancing measures.
Build up capacity
The US (and presumably the UK) are about to go to war without armor.
We have masks for just two weeks, few personal protective equipment (PPE), not enough ventilators, not enough ICU beds, not enough ECMOs (blood oxygenation machines)… This is why the fatality rate would be so high in a mitigation strategy.
But if we buy ourselves some time, we can turn this around:
- We have more time to buy all the equipment we will need for a future wave.
- We can quickly build up our production of masks, PPEs, ventilators, ECMOs, and any other critical device to reduce the fatality rate.
Put in another way: we don’t need years to get our armor, we need weeks. Let’s do everything we can to get our production humming now. Countries are mobilized. People are being inventive, such as using 3D printing for ventilator parts. We can do it. We just need more time. Would you wait a few weeks to get yourself some armor before facing a mortal enemy?
This is not the only capacity we need. We will need health workers as soon as possible. Where will we get them? We need to train people to assist nurses, and we need to get medical workers out of retirement. Many countries have already started, but this takes time. We can do this in a few weeks, but not if everything collapses.
Lower public contagiousness
The public is scared. The coronavirus is new. There’s so much we don’t know how to do yet! People haven’t learned to stop hand-shaking. They still hug. They don’t open doors with their elbow. They don’t wash their hands after touching a door knob. They don’t disinfect tables before sitting.
Once we have enough masks, we can use them outside of the healthcare system too. Right now, it’s better to keep masks for healthcare workers. But if they weren’t scarce, people should wear them in their daily lives, making it less likely that they infect other people when sick, and with proper training also reducing the likelihood that the wearers get infected. (In the meantime, wearing something is better than nothing.)
All of these are pretty cheap ways to reduce the transmission rate. The less this virus propagates, the fewer measures we’ll need in the future to contain it. But we need time to educate people on all these measures and equip them.
Understand the virus
We know very very little about the virus. But every week, hundreds of new papers are coming.
![]()
The world is finally united against a common enemy. Researchers around the globe are mobilizing to understand this virus better.
How does the virus spread?
How can contagion be slowed down?
What is the share of asymptomatic carriers?
Are they contagious? How much?
What are good treatments?
How long does it survive?
On what surfaces?
How do different social distancing measures impact the transmission rate?
What’s their cost?
What are tracing best practices?
How reliable are our tests?
Clear answers to these questions will help make our response as targeted as possible while minimizing collateral economic and social damage. And they will come in weeks, not years.
Find treatments
Not only that, but what if we found a treatment in the next few weeks? Any day we buy gets us closer to that. Right now, there are already several candidates, such as Favipiravir or Chloroquine. What if it turned out that in two months we discovered a treatment for the coronavirus? How stupid would we look if we already had millions of deaths following a mitigation strategy?
Understand the cost-benefits
All of the factors above can help us save millions of lives. That should be enough. Unfortunately, politicians can’t only think about the lives of the infected. They must think about all the population, and heavy social distancing measures have an impact on others.
Right now we have no idea how different social distancing measures reduce transmission. We also have no clue what their economic and social costs are.
Isn’t it a bit difficult to decide what measures we need for the long term if we don’t know their cost or benefit?
A few weeks would give us enough time to start studying them, understand them, prioritize them, and decide which ones to follow.
Fewer cases, more understanding of the problem, building up assets, understanding the virus, understanding the cost-benefit of different measures, educating the public… These are some core tools to fight the virus, and we just need a few weeks to develop many of them. Wouldn’t it be dumb to commit to a strategy that throws us instead, unprepared, into the jaws of our enemy? (To be concluded) – Rappler.com
READ: Conclusion | [ANALYSIS] COVID-19: The hammer and the dance
*Tomas Pueyo is a Silicon Valley entrepreneur and behavioral psychologist who specializes in exponential growth. He wrote the Medium post, "Coronavirus: Why You Must Act Now," which was read by tens of millions of people around the world.
READ Pueyo's previous work:
![]()